Degradation of Visual Acuity upon Removal of Corneal Refractive Therapy Contact Lenses
Marc Masbou
June 9, 2010
Introduction
Most Americans do not see well. In 2007, approximately 76% of Americans needed some form of vision correction [1]. The three most common types of visual defects are hyperopia (farsightedness), myopia (nearsightedness), and astigmatism. Myopia has been increasing at an astounding rate in the past few decades. In the 1970’s, approximately 25% of Americans suffered from myopia, whereas in 2009 that number was 41% [2]. Although the majority of cases of myopia occur early in a patient’s life (between the ages of 8 and 14), 10-50% of cases are classified as adult-onset myopia (taking place after the age of 18) [3].
What is Myopia?
Myopia results when the focusing power of the cornea and lens is too strong. The focal length in the eye is too short, so the image plane is in front (instead of on) the retina (see Fig. 1 below). Conceptually, this problem can be corrected by placing a diverging lens in front of the eye. This lens will push the focal point back onto the retina, resulting in clear vision.
Fig. 1 - Myopia
Photo source: [4]
Options
There are many ways to correct myopia. They can be broken into three main groups: temporary, permanent, and “perma-temp.”
Temporary correction is accomplished by physically placing a diverging lens in front of the eye. This could include corrective glasses or contacts, and is by far the most popular. The benefits of a temporary solution include immediate results, low cost, and simple application. However, the main drawback of these solutions is the fact that their results are transient. Remove the diverging lens, and the patient’s vision returns to its myopic state.
Permanent correction is a surgical procedure in which the visual system in the eye is modified. The most popular form of permanent correction is LASIK, in which the cornea is physically modified to remove myopia. The top layer of the cornea is cut and peeled back, then a high-powered laser is used to reshape the corneal stroma to remove myopia. The top layer is then repositioned, and remains in position by natural adhesion until healing is complete. This is a very complicated surgical procedure, and can potentially result in serious unwanted side effects, including: double vision, fluctuation in visual acuity, dry eyes, glare, and loss of contrast sensitivity [5].
What we have termed “perma-temp” correction is hybrid of temporary and permanent correction. This differs from temporary correction in that when the correcting device is removed, the patient’s vision does not immediately degrade to its previous state. Instead it degrades over time, gradually returning to the patient’s initial state. During this time, the patient enjoys improved visual acuity. Perma-temp is a merely a term coined for this project to better illustrate this technique in comparison to temporary and permanent alternatives; in general this field is known as corneal refractive therapy or orthokeratology.
Corneal Refractive Therapy (CRT)
The main idea behind corneal refractive therapy is to correct the refractive error of the eye by reshaping the cornea in a non-permanent, non-destructive manner [6]. This technique is successful due to the importance of the cornea’s role in refracting light in the eye. The cornea represents between 66% and 80% of the refracting power of the optical system in the eye, whereas the lens represents the remaining minority [7] [8]. In addition to the fact that the cornea represents the majority of the refracting power of the eye, it is the outer layer of the cornea (which interacts with outside air) that generates the majority of the refracting power within the cornea. This has great implications for corneal refractive therapy, as the part of the eye that is easiest to access is also the part that has the greatest refractive power of the optical system.
So how is the cornea reshaped? Corneal refractive therapy is a technique that has existed for hundreds of years, and has evolved over time. “The ancient Chinese placed sandbags on the eyes at night in an attempt to reduce myopia by flattening corneas. In 1850, a Dr. J. Bell developed an eye cup with a spring-mounted plunger that aimed for a similar effect by applying pressure through the closed lid [6]." Corneal reshaping is currently achieved with precise contact lenses. The breakthrough in developing contact lenses for CRT occurred in the 1990’s, and was brought about by the advent of computerized corneal topography, advances in rigid gas permeable lenses, and the introduction of computer-controlled lathes with sub-micron precision [9].
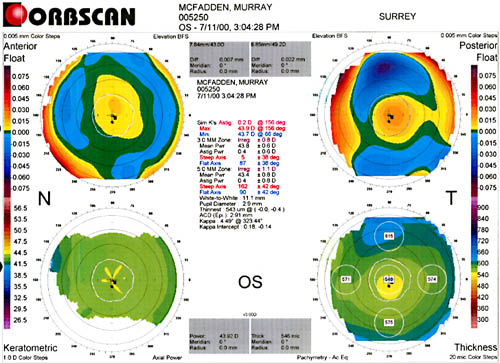
Fig. 2 - Corneal Topographical Map
Photo source: [10]
Together, these advancements meant that contact lenses could be developed that could, while the patient was sleeping, accurately reshape the cornea to correct myopia and astigmatism. The first commercial company to release a CRT product was Paragon, who received FDA approval in 2002 to produce lenses that could correct myopia up to 6 diopters, and astigmatism up to 1.75 diopters [6].
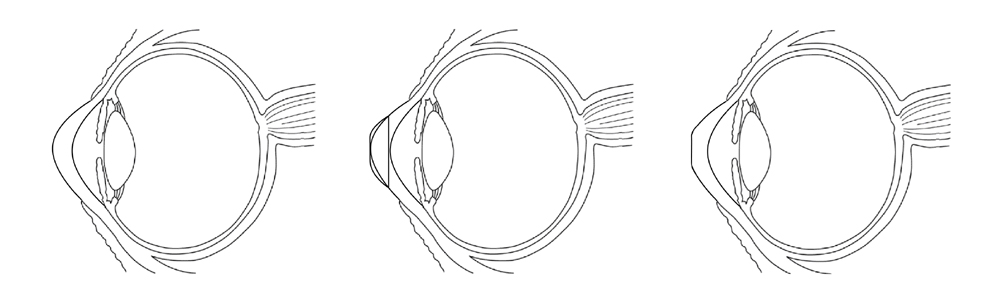
Fig. 3 - Desired Outcome of CRT
Photo derived from: [11]
Paragon’s product has been very successful, with 93% of successful CRT patients having 20/32 or better vision, and 66% having 20/20 or better vision binocularly [12].
Our question
As previously discussed, the results of CRT contact lenses can be described as “perma-temp.” The cornea is reshaped, but after a period of time, it returns to its original shape. This “wash-out” period is usually on the order of one week. We were curious to see how visual acuity degraded over time, as this is related to how often a patient must wear his/her CRT lenses. Most CRT users wear their contacts every night, although some reportedly only need to wear their contacts once every three nights [12]. A Paragon study to examine the variance between patients found that the lasting effect of CRT is dependent upon the patient’s corneal refraction before lens application, as well as immediately after lens removal. After removal, if a patient’s vision is slightly hyperopic, the effects of CRT last longer [13].
Methodology
For the sake of simplicity, Snellen charts were used to gauge the visual acuity of the patient’s eyes. To prevent memorization of any specific chart, 17 randomized Snellen charts were printed and cycled through. Although the traditional Snellen chart uses only letters from a certain set (the 10 Sloan letters), the randomized Snellen charts used for this experiment included letters from the whole alphabet. In addition, the charts used in this experiment differed from traditional Snellen charts in that they only had 8 lines of letters, ranging in size from the equivalent of 20/70 vision to 20/10 vision. The traditional Snellen chart has 11 lines and ranges from the equivalent of 20/200 to 20/4 [14]. Also, it is important to note that the readings were done binocularly, that is, neither eye was covered. A reading was done on average about once an hour (excluding sleeping hours).
Fig. 4 - Snellen Chart
Photo source: [15]
Results
Here are the results over four days of testing.
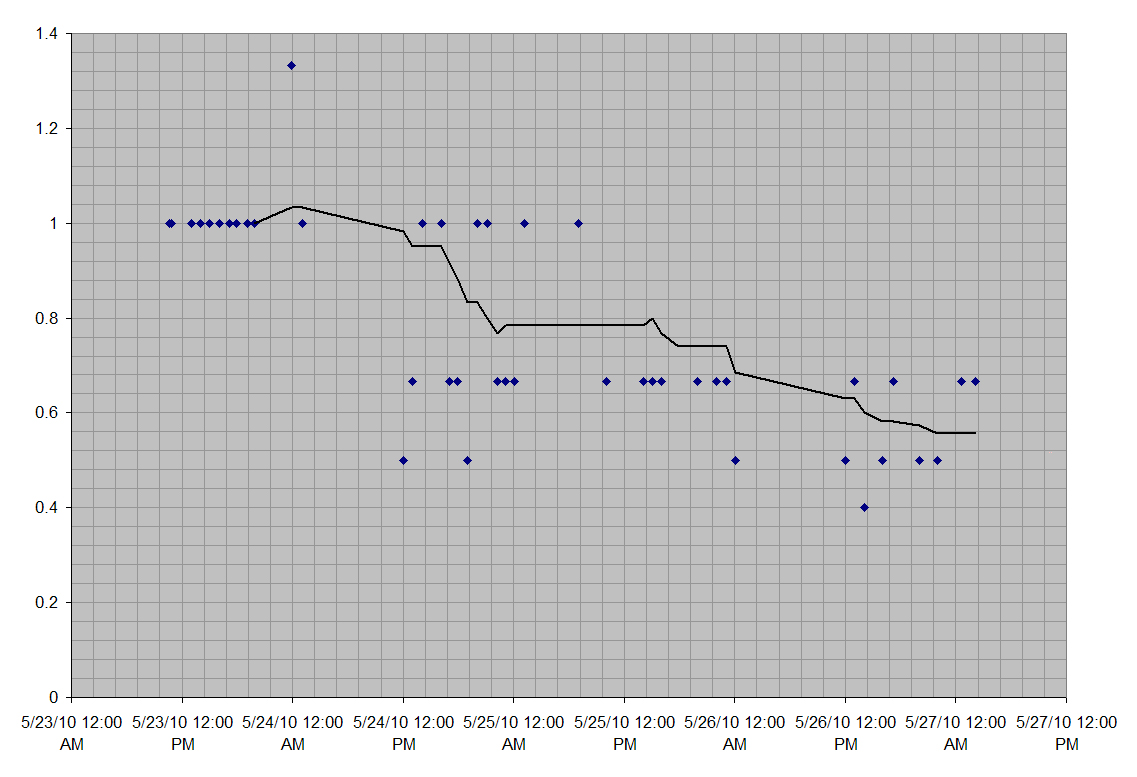
Fig. 5 - Official Snellen Fractions
The Y-axis here is the Snellen fraction. For example, 1 represents the fraction 20/20. The X-axis is the time of the reading. The line shown is the moving average of the results. As can be seen, the moving average degrades fairly linearly over time.
Since these results are severely quantized by the limited number of lines on the Snellen chart, we re-compiled the results instead as the percent of letters that were identified correctly. These results are shown below.
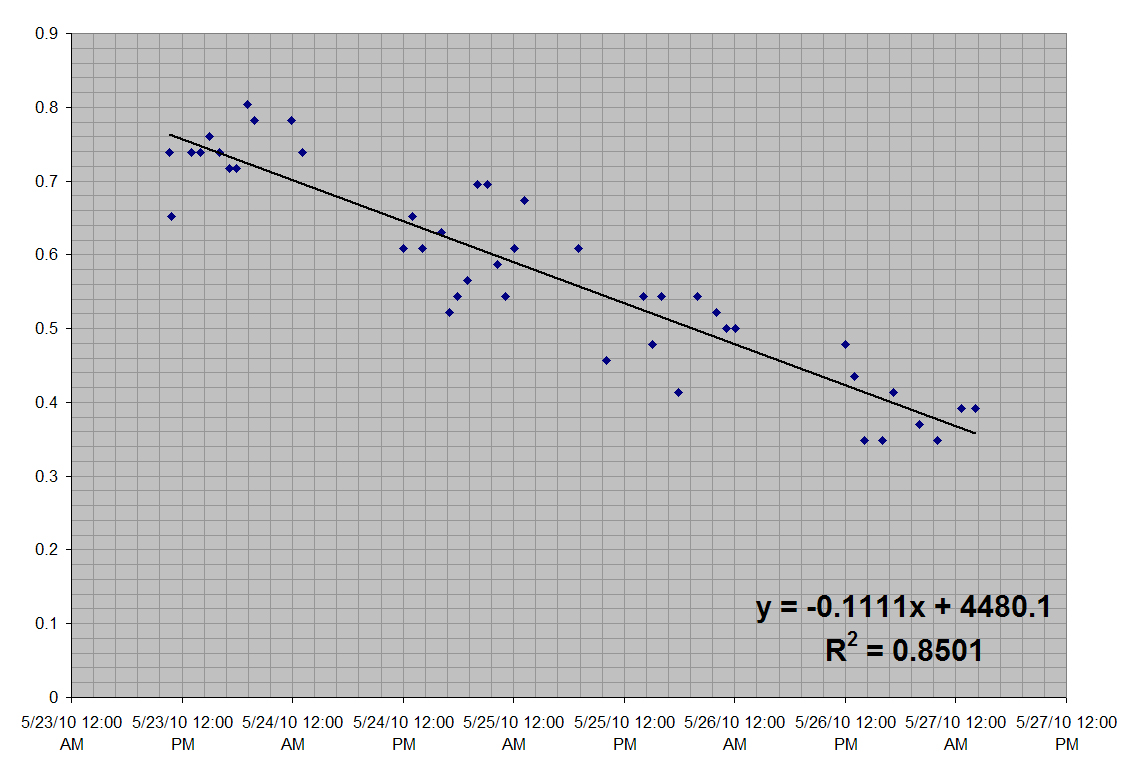
Fig. 6 - Percent Identifiable
Here the Y-axis is the percent of letters identified correctly and the X-axis is time. A linear decrease over time is fairly evident, with an R2 value of 0.8501. Next we split the results by day.
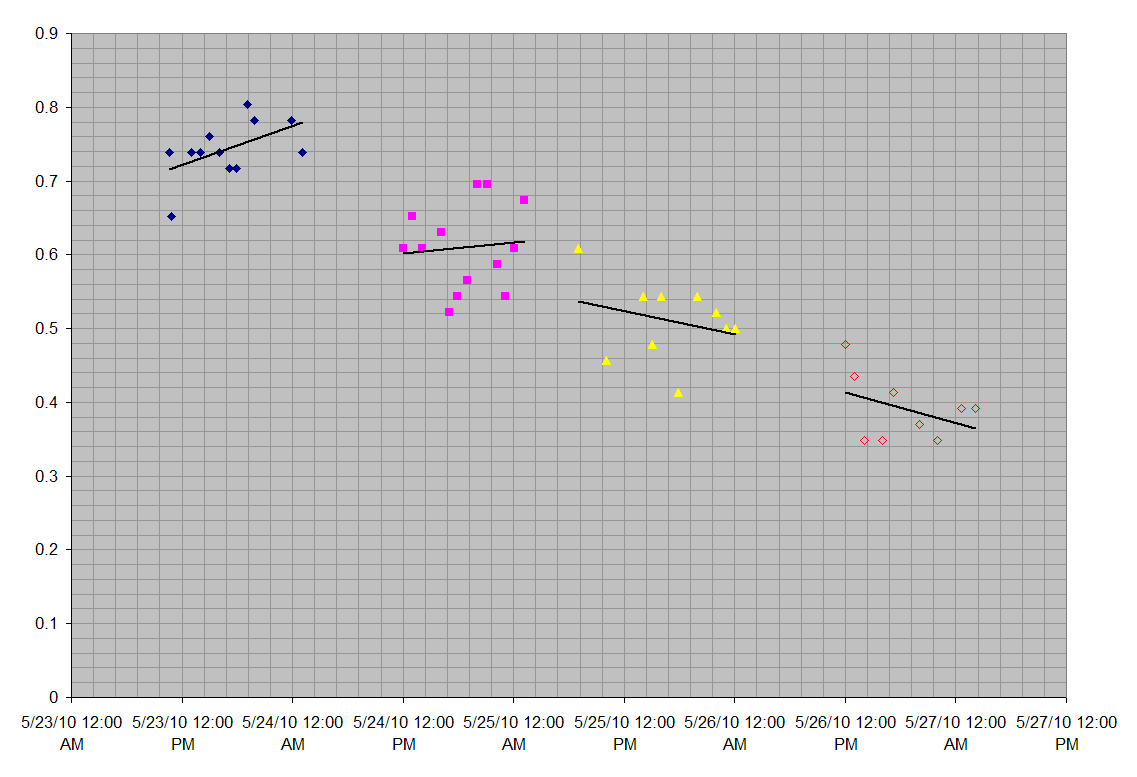
Fig. 7 - Percent Identifiable by Day
This graph shows the same results as in Fig. 6, but split over each day. Interestingly, for the first two days, the percent of letters identified rose throughout the day. On the other hand, the percent of letters identified takes a big drop overnight. This seems to indicate that when the eye is actively being used, the cornea maintains its shape much better than when the eye is relaxed.
Overall, after removing CRT lenses, visual acuity tends to degrade in a linear fashion. The patient’s visual acuity degraded from 20/20 binocularly immediately upon removal, to between 20/30 and 20/40 binocularly, over a period of 4 days.
What’s Next
Our results from this experiment are obviously very preliminary. In the grand scheme of things, Snellen charts are not a good way to measure visual acuity, as processing done by the brain’s visual system plays a huge role in determining the result. An improved experiment would use a setup similar to the one employed by Campbell and Gubisch in their paper ‘Optical Quality of the Human Eye’ [16]. Their setup directly measured the diffraction generated by the cornea and lens in the visual system of the human eye. By using a similar setup, the degradation of a patient’s visual acuity could be measured with much finer granularity. Finally, for convenience’s sake, this experiment was done on a lone patient (the author). It would be interesting to see if the results are consistent over a larger set of patients.
Sources
[1] Vision Monday: Americans Embrace Vision Correction in Larger Numbers.
http://www.visionmonday.com/ViewContent/tabid/211/content_id/2562/Default.aspx
[2] ABCNews.com: Study Finds Many More Nearsighted Americans.
http://abcnews.go.com/GMA/OnCall/nearsighted-americans-texting-partially-blame/story?id=9347796
[3] Dirani, Mohamed, Shekar, Sri N., and Baird, Paul N.: Adult-Onset Myopia: The Genes in Myopia (GEM) Twin Study.
http://www.iovs.org/cgi/content/full/49/8/3324
[4] HyperPhysics: Myopia (Nearsightedness).
http://hyperphysics.phy-astr.gsu.edu/hbase/vision/eyedef.html#c4
[5] Wikipedia: LASIK.
http://en.wikipedia.org/wiki/LASIK
[6] Refractive Eyecare: Corneal Refractive Therapy (CRT): A Valuable Practice Addition.
[7] Wikipedia: Cornea.
http://en.wikipedia.org/wiki/Cornea
[8] HyperPhysics: The Cornea.
http://hyperphysics.phy-astr.gsu.edu/hbase/vision/eyescal.html#c2
[9] Wikipedia: Orthokeratology.
http://en.wikipedia.org/wiki/Orthokeratology
[10] PRK & LASIK Today: Laser Eye Surgery.
http://www.lasik1.com/TopoMap.html
[11] Wikimedia: File:Eye diagram (ja).png.
http://commons.wikimedia.org/wiki/File:Eye_diagram_(ja).png
[12] Paragon Website.
[13] Contact Lens Spectrum: A Closer Look at FDA Contact Lens Labeling.
http://www.clspectrum.com/article.aspx?article=&loc=archive\2003\January\0103044.htm
[14] Wikipedia: File:Snellen chart.svg.
http://en.wikipedia.org/wiki/File:Snellen_chart.svg
[15] Wikipedia: Snellen Chart.
http://en.wikipedia.org/wiki/Snellen_chart
[16] Campbell, F.W., and Gubisch, R.W.: Optical Quality of the Human Eye.