Feasibility of SVM Diagnosis of III/VI Cranial Nerve Palsies and Myasthenia
Kevin Gabayan, kevingabayan gmail com
Psych 221 Class Project, Spring 2010
Stanford University
Neuropathies including III and VI Cranial Nerve Palsies and Myasthenia manifest themselves in disconjugate eye movements and can be detected through inspection of saccadic eye tracking data. To overcome the costs of manual diagnosis, I propose a computer-aided diagnosis to be used as a screening tool for neuropathies. The computer-aided generation and selection of features of eye-tracking data from patients can also aid in the characterization of conditions where its characterization is disputed in the literature. As a feasibility study, synthetic eye tracking data was generated from models of abnormal eye movement conditions and noises to train SVM classifiers. The classifiers performed with >95% accuracy when detecting abnormal eye movements that were beyond 10% reduction from the healthy saccade amplitude, which is expected to sufficiently detect abnormal eye movements from real patient data.
Introduction
One method of indentifying patients of the Eye Clinic as candidates for neuropathies is the inspection of their eye tracking data. If manual inspection of eye tracking data reveals telltale signs of a neuropathy, the patient may be referred to more specific diagnostics.
The eye tracking setup at the Eye Clinic is as follows:
We use the visual stimulus program Presentation running on a Windows XP laptop to generate a visual stimulus that is displayed on a LCD monitor. A typical patient is presented with a range of stimuli to induce saccades and smooth pursuits exercising the range of a patients eye movement in randomized directions, as well as reading and image inspections. The iView X Hi-Speed Eye Tracker is an eyetracker using the IR video-oculography technique to recover binocular point-of-regard with a sampling rate of at most 500 Hz.
Figure 1. The SMI iView X HiSpeed eye tracker. [
Image link]
A patient views the monitor through the eye tracker column while the stimulus is being displayed, and an eye tracking waveform is saved by the computer. An ophthalmologist may then manually inspect plots of the eye tracking data to perform a diagnosis. Some telltale symptoms of some common conditions for patients visiting the clinic are manifested in saccadic eye movements and include:
|
Condition
|
Symptoms manifested in saccades
|
|
III Cranial Nerve Palsy
|
Roughly equal reduction of saccadic amplitudes and velocities in both horizontal and vertical directions
|
|
VI Cranial Nerve Palsy
|
Reduction in saccadic amplitude and velocity in abduction
|
|
Myasthenia
|
Fatigue in repeated saccades in abduction
|
The effect of some conditions on saccades, including Thyroid Eye Disease, is still disputed in the literature.
Proposed Method
I propose a computer-aided diagnosis for the above symptoms. A simple approach can involve detecting the above symptoms of amplitude and velocity reduction as heuristics to diagnose a condition. However, these heuristics alone are of disputed efficacy in the diagnosis of some conditions including Thyroid Eye Disease. Data mining techniques may discover new features of eye movement that indicate these conditions more powerfully than traditional amplitude and velocity thresholding. Thus, amplitude and velocity thresholding will not be explored in this classification, but can be used as a feature in a classifier's feature vector.
The computer-aided diagnosis is not intended as a substitute for an ophthalmologist's diagnosis but is intended to augment the set of diagnostic tools used under an ophthalmologist's supervision. By exhaustively analyzing eye tracking data from a patient, such a system can:
. Enable the diagnosis of more conditions faster
. Reduce costs
. Generate quantitative digital evidence of abnormal symptoms
. Generate datasets required to resolve disputes in the characterization of neuropathies
A data mining approach does require a large amount of data to prove statistical significance. To build classifiers for each of the conditions mentioned above that are manifested in saccades, we will need a large amount of exemplar saccades from normal and abnormal patients. Saccade recordings are included in the eye tracking protocol given to many patients visiting the Stanford Eye Clinic, but few if any recordings per patient exists for each saccade direction, and many of these are corrupted by artifacts due to head motion or blinking. The system we use does not detect head motion or blinking artifacts in real-time nor does it display data during recording such that artifacts can be manually detected in real-time, so detection of these artifacts upon viewing the data more often occurs after the patient has left the clinic, prohibiting the ease of re-recording the patient. Our archived dataset of eye tracking traces from Stanford Eye Clinic patients contains few recordings free of artifacts in each of primary eye movement directions, and unfortunately we will have to revert to synthetic eye tracking data and test only the feasibility of our classification approach.
Synthetic Eye Tracking Data
Synthetic eye movement waveforms were generated based on specifications in existing saccadic eye movement literature.
A saccade waveform recorded by our eyetracker records the eye's point-of-regard (in display coordinates) over time. Considering the display conditions in the clinic we can solve visual angle from monitor point-of-regard. For example, the horizontal angle waveform of an abducting saccade records the viewing angle as it:
1) fixates on its first position
2) accelerates to a peak velocity and decelerates to its second position
3) fixates on its second position
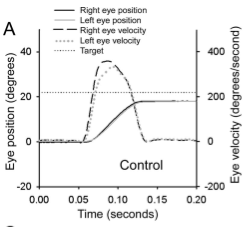
Figure 2. On the left is a prototypical normal saccade shown in the paper of Serra, et al [1]. On the right is a plot of a normal saccade recorded from the Eye Clinic, which is consistent with the prototypical shape from Serra et al.
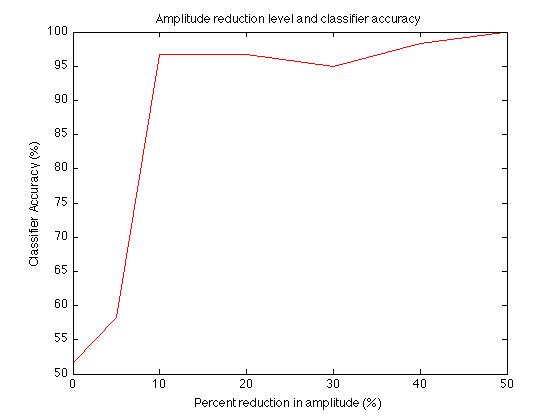
Peak saccade velocity can also be approximated as a linear function of target angle [2]. A linear fit to typical peak saccade velocities and target angles produced the following mapping:
The eye tracker recording noise has been modeled as additive zero-mean Gaussian noise with a standard deviation of 0.3 degrees of visual angle.
Modeling Conditions
The abnormal eye movement conditions of interest were modeled as reductions of peak saccade amplitude and velocity. Eyes were modeled as having peak saccade amplitudes and velocities, and abnormal conditions were modeled as reductions on these peak velocities. Fatigue was modeled as a further reduction of these peak values as an effect of repeated trials.
Peak amplitude and peak velocity properties were stored for each cardinal direction {up, down, left, right} of eye movement for a virtual eye. Reduction factors were chosen for each condition based on the prototypical pathological eye traces from Serra's paper [1]:
|
Condition
|
Mean Reduction Factors
|
|
III Cranial Nerve Palsy
|
Roughly equal reduction of saccadic amplitudes and velocities in both horizontal and vertical axes
|
|
VI Cranial Nerve Palsy
|
66% reduction in saccadic amplitude and velocity in abduction
|
|
Myasthenia
|
Fatigue in repeated saccades in abduction, for example, 10% amplitude and velocity reduction
|
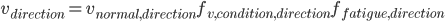
When generating a synthetic waveform for a particular virtual eye, the amplitudes and velocities for each cardinal direction were selected as a product of the normal parameter and reduction factors due to abnormal conditions and fatigue:
Synthetic Waveforms
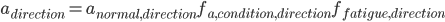
Figure 3. Synthetic saccade waveforms with fitted curves. The left eye is exhibiting a 66% reduction in adduction saccade amplitude.
Patients were modeled with two eyes: one normal eye and one eye with their condition. The normal patient had two normal eyes, while the III and VI CN palsy and Myasthenia patients had one normal eye and one weak eye. Synthetic binocular eye tracking waveforms were generated from a given saccade stimulus, approximated as a piecewise linear function smoothed with a boxcar averaging filter and corrupted with Gaussian noise. This is a coarse approximation, ignoring finer transient oscillations and high frequency tremors and microsaccades present in real eye tracking data. In each eye the actual reduction factors of amplitude, velocity, and fatigue are randomly selected from a Gaussian distribution centered about the approximate mean values for each condition. In each trial, the peak amplitude and velocity of the saccade is also selected from a Gaussian distribution centered at their computed mean values, to assert that our synthetic trials are unique.
The onset of the saccade has been chosen to follow the stimulus onset following a fixed noticing delay, and the eye position accelerates to peak velocity and plateaus to reach its target value. In the event that the target value is greater than the limits of the eye model due to an abnormal eye condition or fatigue, the eye position will plateau at its maximum value.
Classification
We have chosen polynomial coefficients to reduce the waveform into a feature vector for classification. Since the stimulus timing, stimulus amplitude, and recording duration is under our control, we can expect that the polynomial coefficients will be sensitive to changes in the patient's condition.
For the III Cranial Nerve palsy condition, 30 traces were generated for the normal condition and 30 traces were generated for the abnormal condition for training data. Similarly, 60 traces containing 50/50 normal/abnormal data was generated as testing data. The 8th order polynomial coefficients of each training waveform was computed, and a label of -1 was applied if it was normal and +1 if it was abnormal. The training data was input to a Matlab interface to libsvm, an open source SVM program, specifying default parameters and a linear training kernel.
Results
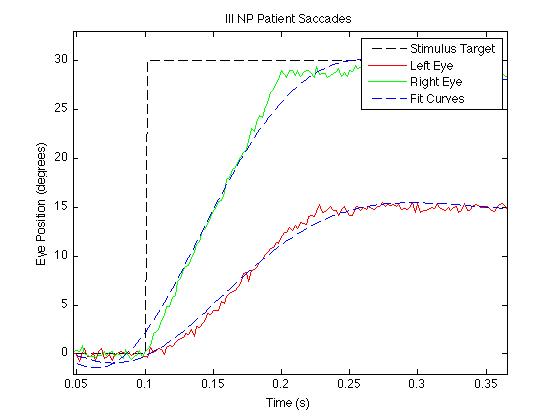
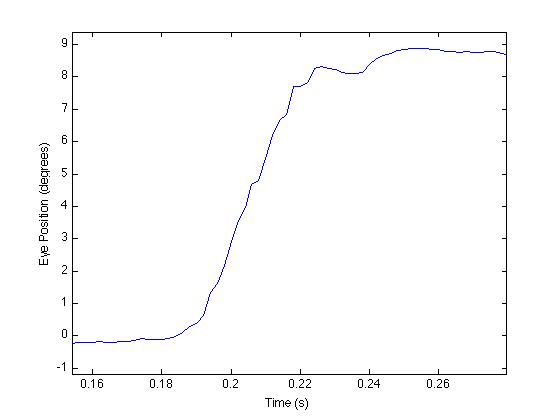
To visualize the effect of the reduction factor on class separability, I've plotted classifier accuracy against saccade amplitude reduction factor for the III CN palsy classifier:
Figure 4. Classifier accuracy vs. Percent reduction in abnormal eye movement amplitude.
Classifier accuracy is successful at >95% accuracy for reduction factors >10%. A reduction factor of 10% corresponds to saccades falling 3 degrees below the normal saccade amplitude. Since prototypical VI CN palsy saccades from Serra's paper exhibit a 66% reduction in saccade amplitude [1], our classifier sensitivity is well above that required to detect these neuropathies and we can expect that our SVM classification method will succeed to detect neuropathy symptoms on real patient data.
Future Work
The next steps in implementing this system are:
. Collect repeated trials of horizontal and vertical saccades to build a dataset from which training and testing dataset may be generated.
. Validate classifier performance on the testing dataset and new patient recordings.
Viewing Conditions
Eye tracker: SMI iView X HiSpeed
Stimulus display: NEC MultiSync 70GX2
Display driving laptop: Sony VAIO VGN-T140P netbook (Pentium M 1.10 Ghz with 512 MB RAM)
Monitor (approximate): 17 inch diagonal, 13 3/8 inch x 10 5/8 inch
Viewing distance (approximate): 20 inches, 2.25 inches from top edge of the display
References
[1] Serra, Liao, Matta, Leigh, "Diagnosing Disconjugate Eye Movements," Neurology October 7, 2008; 71: 1167-1175.
[2] Wikipedia, "Saccade," Website accessed June 1, 2010. http://en.wikipedia.org/wiki/Saccade
![v(\theta) = 10\theta + 200 \;\;\; [\;\;^{\circ}/s ]](images/EXTERN_0000.png)